This is the second and final part of a blog-post where I’d like to take the opportunity to shed some light on what the findings from my study might mean for practising clinicians by addressing questions/comments that have been directed to me that have appeared in social media. By necessity some of the questions/comments are paraphrased and I have tried hard not to misinterpret these. I’m only too happy to (try to) answer any further questions you might have as a result of reading these posts. Please post comments, especially if you disagree! (Although please be polite! It’s fine to attack methods and methodology, not people). The limitations of the study should always be kept in mind when interpreting the ‘clinical implications’ responses to each comment. I look forward to hearing from you!
Comment 3 – ‘[Would have been] more interesting/important to research cervical inter-vertebral rotation in the transverse plane’
This study investigated cervical inter-vertebral flexion-extension (angular rotation in the sagittal plane) as it is not currently possible to use quantitative fluoroscopy to measure inter-vertebral rotation (angular rotation in the transverse plane) or lateral flexion (angular rotation in the coronal plane) due to radiographic superimposition. Axial rotation motion has been measured using CT and biplanar radiography (Bogduk and Mercer 2000) but accuracy can be problematic and radiation doses are high (Anderst et al. 2011).
I agree that, based on clinical experience, it would be interesting to measure inter-vertebral motion during regional rotation. What might make this possible one day is the creation of 3-D models of patients’ spines by combining MRI data with the continuous inter-vertebral motion data provided by quantitative fluoroscopy – but this is probably a long way off! Until measurement methods improve it will not possible to measure the effects of SMT on inter-vertebral motion other than in the sagittal plane (flexion-extension).
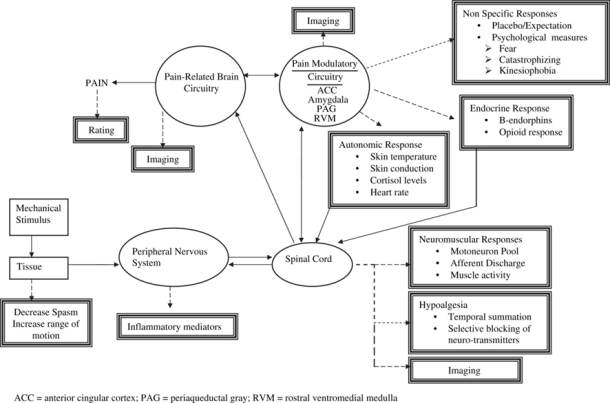
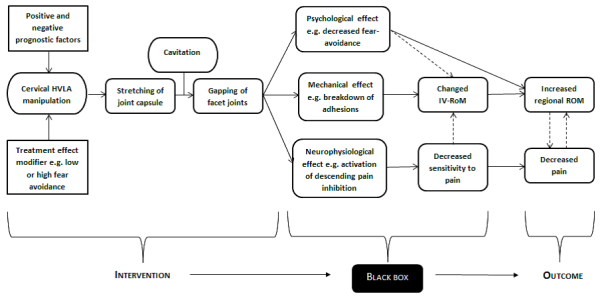
It should also be noted that changes in passive regional cervical ROM after SMT have been found to only be short-term (Nilsson et al. 1996). It is worth also considering the other factors at play as suggested in the diagram below:
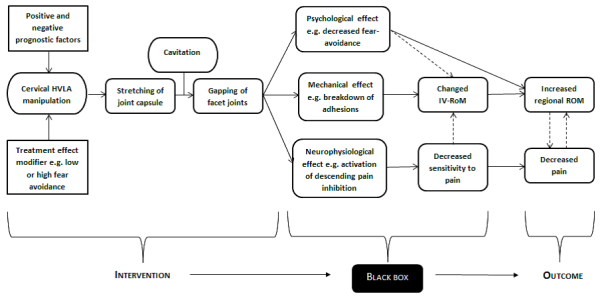 The ‘black box’ represents the (unknown) underlying mechanisms that account for the outcome after an intervention (Howick et al. 2010). In the above black box are mechanical, neurophysiological and psychological effects (mechanisms) that may be considered to act in isolation or in concert in producing the clinical outcome. ‘Changed IV-RoM’ includes the possibility of a change (increase) in range, or change in another kinematic variable, e.g. IAR location, with or without a change in range.
The ‘black box’ represents the (unknown) underlying mechanisms that account for the outcome after an intervention (Howick et al. 2010). In the above black box are mechanical, neurophysiological and psychological effects (mechanisms) that may be considered to act in isolation or in concert in producing the clinical outcome. ‘Changed IV-RoM’ includes the possibility of a change (increase) in range, or change in another kinematic variable, e.g. IAR location, with or without a change in range.
Figure 4: A suggested mechanistic chain to explain the clinical effects of spinal manipulative therapy (Branney 2015)
Clinical implications? – Current methods only allow for measurement of inter-vertebral angular rotation in the sagittal plane (flexion-extension). Other factors that can influence patient recovery, or otherwise, (Figure 4) should also be considered.
Comment 4 – ‘If there is no difference in intervertebral movement between those with and those without neck pain and we can’t palpate with reasonable certainty which joints are “locked”, and we can’t effect intervertebral ROM and movement with SMT, then why use time on this?’
Good point – doesn’t sound good when you put it like that! It should be said that the findings from my study are not definitive, mainly through it having a small sample size (29 patients, 30 healthy volunteers). Also, the patients in the study were of low/moderate disability – there might be important inter-vertebral motion differences in patients of high neck pain-related disability. Further, differences may not be detected in terms of ROM but other parameters might be important such as IAR (instantaneous axis of rotation) that future studies could measure. However, this doesn’t stop palpation being problematic with studies consistently finding this is not reliable for assessing motion alone; the presence of pain however increases reliability.
Clinical implications? – In the absence of pain it is possible that inter-vertebral motion is not clinically important, or at least we are as yet unable to measure clinically important inter-vertebral motion abnormalities.
Comment 5 – ‘Perhaps it is something else than intersegmental hypomobility we palpate, but should still continue with motion palpation?’
This links with comment 4 and begs the question, if motion palpation is not reliable, what are we feeling when we palpate patients’ spines, and it feels like a joint is restricted? Could we be palpating anisotropic muscle? Might this respond favourably to SMT? We’re back to considering neurophysiological mechanisms…
In Conclusion…
I have attempted to address a number of comments that were made in social media discussions of my PhD study’s findings. I hope I have not misinterpreted any of these comments. My responses may have opened more questions than provided answers and I’d be really interested to hear from anyone who would like to add their thoughts which may include disagreement with any of the above. Any more questions regarding my PhD study are most welcome. I’d also like to point out this study would not have been possible without the fantastic support of Professor Alan Breen and that of my other supervisors, Professor Jenni Bolton and Associate Professor Sarah Hean. Thank you very much again.
An overall conclusion is that we still do not understand how SMT works but I’d like to finish on this note: despite whatever mechanism SMT works by (see Figure 4), 87% of patients in the study had clinically meaningful decreases in pain and disability, and I’m sure that’s all the patients cared about.
References
Anderst, W. J., Baillargeon E., Donaldson, W. F., Lee, J. Y. and Kang, J. D., 2011. Validation of a noninvasive technique to precisely measure in vivo three-dimensional cervical spine movement. Spine, 36 (6), E393-E400.
Assendelft, W. J. J., Bouter, L. M. and Knipschild, P. G., 1996. Complications of spinal manipulation: A comprehensive review of the literature. The Journal of Family Practice, 42 (5), 475-480.
Bialosky, J. E., Bishop, M. D., Price, D. D., Robinson, M. E. and George, S. Z., 2009. The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Manual Therapy, 14, 531-538.
Bogduk, N. and Mercer, S., 2000. Biomechanics of the cervical spine, I: Normal kinematics. Clinical Biomechanics, 15, 633-648.
Branney, J. (2015) An observational study of changes in cervical inter-vertebral motion and the relationship with patient-reported outcomes in patients undergoing spinal manipulative therapy for neck pain. PhD Thesis, Bournemouth University. (not yet published)
Coronado, R. A., Gay, C. W., Bialosky, J. E., Carnaby, G. D., Bishop, M. D. and George, S. Z., 2012. Changes in pain sensitivity following spinal manipulation: A systematic review and meta-analysis. Journal of Electromyography and Kinesiology, 22 (5), 752-767.
Deitz, A. K., Breen, A. C., Mellor, F. E., Teyhen, D. S., Panjabi, M. M. and Wong, K. W. M., 2011. Kinematics of the Aging Spine: A Review of Past Knowledge and Survery of Recent Developments, with a Focus on Patient-Management Implications for the Clinical Practitioner. . In: Yue, J. J., Guyer, R. D., Johnson, J. P., Khoo, L. T., and Hochschuler, S. H., eds. The Comprehensive Treatment of the Aging Spine: Minimally Invasive and Advanced Techniques. 1. Philadelphia: Saunders, 51-62.
Howick, J., Glasziou, P. and Aronson, J. K., 2010. Evidence-based mechanistic reasoning. Journal of the Royal Society of Medicine, 103 (11), 433-441.
Kingston, L., Claydon, L. and Tumilty, S., 2014. The Effects Of Spinal Mobilizations On The Sympathetic Nervous System: A Systematic Review. Manual Therapy, 19 (4), 281-287.
Martinez-Segura, R., De-La-Llave-Rincon, A. I., Ortega-Santiago, R., Cleland, J. A. and Fernandez-De-las-Penas, C., 2012. Immediate changes in widespread pressure pain sensitivity, neck pain, and cervical range of motion after cervial or thoracic thrust manipulation in patients with bilateral chronic mechanical neck pain: A randomized clinical trial. Journal of Orthopaedic & Sports Physical Therapy, 42 (9), 806-814.
Meier, M. L., Hotz-Boendermaker, S., Boendermaker, B., Luechinger, R. and Humphreys, B. K., 2014. Neural responses of posterior to anterior movement on lumbar vertebrae: a functional magnetic resonance imaging study. Journal of Manipulative & Physiological Therapeutics, 37 (1), 32-41.
Nilsson, N., Christensen, H. W. and Hartvigsen, J., 1996. Lasting changes in passive range of motion after spinal manipulation: a randomised, blind, controlled trial. Journal of Manipulative & Physiological Therapeutics, 19 (3), 165-168.
Padayachy, K., Vawda, G. H. M., Shaik, J. and McCarthy, P. W., 2010. The immediate effect of low back manipulation on serum cortisol levels in adult males with mechanical low back pain. Clinical Chiropractic, 13 (4), 246-252.
Pickar, J. G. and Bolton, P. S., 2012. Spinal manipulative therapy and somatosensory activation. Journal of Electromyography and Kinesiology, 22, 785-794.
Song, X. J., Gan, Q., Cao, J. L., Wang, Z. B. and Rupert, R. L., 2006. Spinal manipulation reduces pain and hyperalgesia after lumbar intervertebral foramen inflammation in the rat. Journal of Manipulative & Physiological Therapeutics, 29 (1), 5-13.
Teodorczyk-Injeyan, J. A., Injeyan, H. S. and Ruegg, R., 2006. Spinal manipulative therapy reduces inflammatory cytokines but not substance P production in normal subjects. Journal of Manipulative & Physiological Therapeutics, 29 (1), 14-21.
Teodorczyk-Injeyan, J. A., Triano, J. J., McGregor, M., Woodhouse, L. and Injeyan, H. S., 2011. Elevated production of inflammatory mediators including nociceptive chemokines in patients with neck pain: a cross-sectional evaluation. Journal of Manipulative & Physiological Therapeutics, 34 (8), 498-505.
Tuchin, P. J., 1998. The effect of chiropractic spinal manipulative therapy on salivary cortisol levels. Journal of Australasian Chiropractic and Osteopathy, 7, 86-92.
Whelan, T. L., Dishman, J. D., Burke, J., Levine, S. and Sciotti, V., 2002. The effect of chiropractic manipulation on salivary cortisol levels. Journal of Manipulative and Physiological Therapeutics, 25 (3), 149-153.


 The ‘black box’ represents the (unknown) underlying mechanisms that account for the outcome after an intervention (
The ‘black box’ represents the (unknown) underlying mechanisms that account for the outcome after an intervention (